-
1. How to Fax an RFA in 30 SecondsSchedule a Call
Say goodbye to manual form fill-outs, and fax compliant RFAs to claims administrators in 30 seconds or less.
-
2. Claims Administrator RFA Fax NumbersSchedule a Call
daisyAuth knows and tracks fax numbers for more than 200 claims administrators in California. With this information at your fingertips, faxing RFAs is a snap.
-
3. Seamless UR Decision TrackingSchedule a Call
Access RFA and UR information with confidence. daisyAuth tracks RFAs and UR decisions for every injury and itemizes the critical details for each requested treatment.
-
4. Easily Send UR Decisions With Your BillsSchedule a Call
Submitting UR documentation with each bill as proof of authorization is mandatory – and daisyAuth technology makes it a breeze.
-
5. daisyAuth Tasks Keep Your Team EfficientSchedule a Call
daisyAuth alerts your team to holdups in the authorization process, from missing documents to overdue UR decisions, and guides you through each step.
-
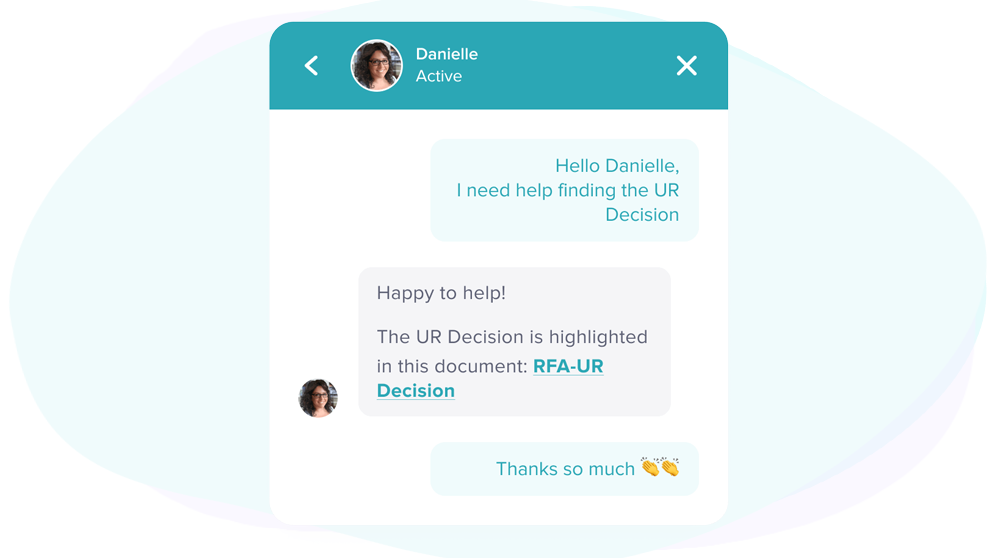 Expert Live HelpSchedule a Call
Expert Live HelpSchedule a CalldaisyAuth experts answer your questions via live chat. Think of us as an (incredibly knowledgeable) extension of your team.